IMPROVE MY GAME
Articles
How To Overcome Golf Injuries And Get Back To Playing Your Best

Injuries in amateur golf are very common. Each year between 15-41% of amatuer golfers report an injury. 31-90% of professional golfers report an injury annually. Professional numbers are higher due to their much higher practice and play volumes. The most common site of injury is the lower back accounting for 18-36% of injuries. The elbow, wrist, hand, and shoulder are also common injury areas.1
(Numbers vary depending on which studies you read, the ones above are taken from a review of a number of papers).
The vast majority of these issues are overuse in nature. This occurs when an area is exposed to a stress it cannot tolerate, over a period of time. A great description of this was outlined in Scott Dye's paper about “the envelope of function” and tissue homeostasis.2 Many of these common golf injuries are not particularly complicated, and can be comprehensively rehabbed if some basic principles are applied consistently. Before getting into what I have found is a useful framework to follow for “run of the mill” aches & pains, let’s look at some reasons why these niggly injuries can hang around for longer than necessary.
From my observations communicating with 1000’s of golfers there are a number of reasons why simple injuries are not well managed, which is hugely affecting the length and quality of recovery for the average case.
- Solely relying on doctors for injury advice: Your family doctor is a terrific resource for managing acute and chronic illness, but probably not the best choice for assessing, diagnosing, and prescribing a plan to overcome an injury and return to sport or high level athletic activity. This is not a knock on doctors, it’s just not a general physician's expertise. The best case scenario is they refer you to a TPI Certified Medical Professional, who you could have just went to in the first place (I understand insurance comes into it for some people). Too often the advice from a physician is extremely conservative, such as “rest” from all activity for a number of days / weeks, ice, anti-inflammatories, and to not lift anything above some arbitrary weight like 5 / 10 / 20lbs. Going to a doctor for injury advice is like going to a physiotherapist for a fever. There are far better options for advice on diagnosis and rehabilitation of a sports related injury. This is not an attack on doctors, it’s just simply not an area of expertise for your general physician / practitioner. (Of course there are some medical doctors who have excellent knowledge in these areas. They are likely specialist consultants however, and extremely expensive.)
-
Concentrating on the symptom rather than improving the situation which lead to the cause: Anti-inflammatories, ice, heat, many passive treatments, and avoidance of loading or stressing the area (often termed as rest) will likely help with short term relief, but are doing little to help prevent the issue from recurring when you resume to normal activity. To prevent the issue recurring when we return to activity we need to build a greater tolerance and conditioning level than was present when the injury originally reared its head.
-
The “I’m fragile” mindset:
S&C professionals have heard every excuse:
“With my bad back I can’t lift that”
“I need to mind my knees”
“That looks like it’s a lot of stress on the _____________”
“I was told I can’t do that anymore”
“At my age………….”
When you have an injured area you have two choices.
Option 1: Gradually train the area and surrounding areas to improve function (mobility strength, power, endurance, etc)
Option 2: Avoid training the area, leading to it getting weaker, more deconditioned and losing function.
Which do you think is better for your long term outcome?
I hope you picked Option 1. So often people choose to do just the opposite. An extremely common scenario I come across is somebody tells me their back or knee hurts during or after playing golf and it’s affecting their performance, enjoyment, or how regularly they can play or practice. I ask them what they’re doing to rectify the situation. They proceed to tell me the usual list of icing or heating, pain killers, wearing a brace / support, resting, and maybe some undirected stretching or massage. The above can be useful for managing the symptoms, but are very unlikely to lead to successful rehabilitation as they do little to nothing for improving long term function.
If you would like to read more about why mechanical stress is essential for tissue health the paper “Optimal Loading: Key Variables & Mechanisms” Glasgow et al (2015) may be of interest to you.3
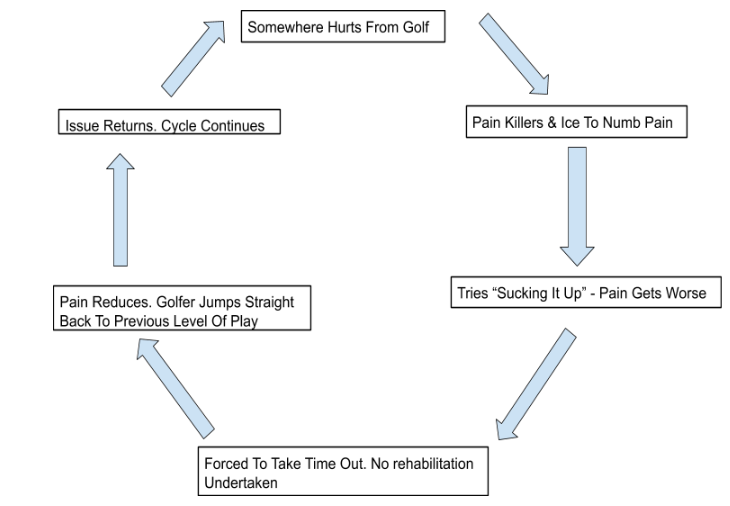
Does This Cycle Of Event’s Sound Familiar?
Golfer’s explain the following cycle to me regularly. Let’s use the shoulder as an example.
- Golfer develops pain in shoulder from golf (can substitute any activity).
- Golfer takes pain killers and uses ice to numb pain.
- Tries “sucking it up” and continues playing the same amount. Shoulder pain gets worse.
- Golfer is forced to take a complete break from golf and decides shoulder needs to “rest”, so stops all activity that load the shoulder.
- Shoulder pain seems to reduce and feels “OK”, golfer jumps straight back into the previous level of activity thinking / hoping shoulder is “fixed”
- Shoulder pain returns.
- Cycle continues.
The diagram below shows an illustration of this. Are you familiar with this cycle?
Cycle Of Recurring Injury In Golfers
Why Don’t You Get Better?
A crucial error many people make when returning to golf after a lay off due to injury (this applies to any activity) is that they bring the previously injured and deconditioned body / body part immediately back to the exact same amount of practice and play that lead to the issue in the first place. This is completely nonsensical. If your tolerance to the stresses of practice and play was below the level needed for your amount of practice and play before the injury, how on earth do you expect the now weaker and more deconditioned area to tolerate the same demands imposed on it?
Although after your rest period the area is no longer sore, this by no means signifies it’s ready to return to your previous volume of practice and play.
You need a structured and progressive rehabilitation plan which improves the loading capacity your body can tolerate. In simple terms this means you probably need to improve your mobility, get stronger and more powerful, and improve your muscular endurance. This doesn't mean that a rehab plan won't include ice, heat, pain killers, massage, cupping, acupuncture, adjustments, needling etc to help address acute pain, but those tools are unlikely to improve an athlete's long-term durability on their own. As TPI likes to say, treat the cause of pain, not just the site of pain.
Khan & Scott (2009) “How Physical Therapists Prescription Of Exercise Promotes Tissue Repair” provides a framework for the importance of mechanotherapy, the process by how load may be therapeutically used to “stimulate tissue repair and remodelling in tendon, muscle, cartilage, and bone”.4
A Better Approach:
An overuse injury is a sign that something needs to change. “Sucking it up” and popping pills is not the long term solution, especially if you care about your body and golf performance.
The first step is something that most golfers do not like to hear. You will need to reduce your practice and play to a level that you can tolerate. This doesn’t mean you have to stop playing golf completely (although it might for a period), but you will need to make some modifications. Exactly what those modifications are and how severe they need to be are impossible to say. There’s many variables and individual nuance that come in to play. In simple terms we need to reduce the type and amount of stress (e.g hitting golf balls) that are the main aggravating factors. Some examples of how to do this include but are not limited to:
-
Playing 9 holes rather than 18.
-
Getting a small bucket of balls rather than large.
-
Changing the surface you hit off when practicing.
-
Doing 2 x 30 minute practice sessions with a couple of days between them, instead of 1 x 60 minute session at once.
-
Working more on short game or less than full speed swings, as opposed to regular long game work.
If we go back to the common cycle I highlighted above, here is a better approach:
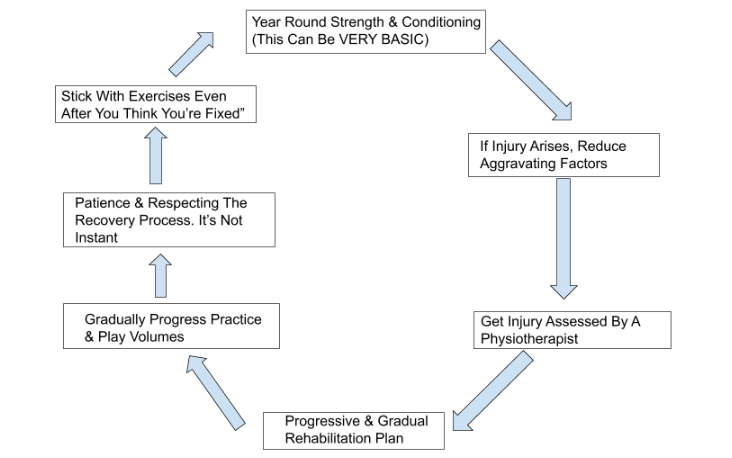
- Golfer performs year round strength & conditioning which hugely reduces chance of picking up an injury. Something as little as 20-30 minutes 2-3 times per week would make a big difference. This can be planned in accordance with your playing amounts at different times of the year.
- If a golfer develops a problem playing golf, they stop “picking the scab” and applying the same stress to the area that is causing aggravation.
- They get the area assessed by somebody experienced in dealing with sports related injuries, AND competent in creating a structured, progressive rehabilitation plan. A comprehensive plan should include exercises based on their assessment, and a discussion on how to GRADUALLY to return to golf. It’s highly unlikely you are getting this from a General Physician. A TPI Medical Professional will likely be the best option for diagnosis. Make sure they have experience dealing with sports related injuries. Either them or a Strength and Conditioning Coach will be best for prescribing a rehabilitation plan. Once you are out of the early stages of rehabilitation a Strength and Conditioning coach will be the best option for creating a long term training program. Medical professionals and Strength and Conditioning coaches often work together with the medical professional being the lead in the early stages of injury & rehabilitation while the Strength & Conditioning Coach has more expertise in guiding the client back to high level performance. The golf coach is applicable should also be involved in this process.
- As your symptoms and function improve the rehabilitation plan should gradually be progressed. It’s important not to rush in this stage. This stage is where many golfers get impatient and just pop some pain killers, get the ice pack, and return to their normal routine, and the same symptoms reappear. After a couple of rehab sessions and a short period of time they throw in the towel and declare “it’s not working”. What they don’t respect is that the issue was created over a long period of time, and it’s foolish to think improvements will be instant.
- As the symptoms and function improve further, gradually build back towards normal practice and play volumes. DO NOT think you’re “fixed” and ditch your exercises. It’s important to remember you need to build up to a level of conditioning that’s higher than the level you were at when the injury presented itself in the first place. Use aggravation as your guide. Some tenderness / soreness / symptoms are to be expected, but they should be mild. If you need to dial it back a little bit, do. Again, the key here is that you don’t revert to complete inactivity, but to the stage of rehab and practice / play that is your “sweet spot”. This is a level that is enough to stimulate recovery and enhancement, but not so much it causes backwards steps.
- Eventually you should be back to better than what you previously considered ‘normal”, and able to withstand more practice and play than you previously would have without having issue.
- I strongly encourage you perform basic year round strength & conditioning training to help prevent these issues arising in the first place. It also hugely improves general physical function and golf performance potential.
Many people don’t have this level of patience, but it’s what’s usually required. It’s a key difference I’ve seen in the attitude of high level athletes who respect their body, the recovery process and want to be better in the long term, versus those looking for a quick fix and masking of symptoms.
(PS If someone is promising a “quick fix” or not advocating progressive structured rehab, beware)
As Charlie Weingroff says “Training = Rehab, Rehab = Training”
A wise approach to this is to start a training program at an appropriate level, taking into account the current state of your injury, function and tolerance level, and level of overall conditioning. You can set a future goal performance level and gradually work towards there.
Many golfers see injuries as isolated issues. They have a sore elbow, back, or shoulder and don’t realise that a better overall level of conditioning will likely make a huge difference to their ability to play and practice without having to deal with these aches and pains.
It’s important for people who are dealing with long term niggles to understand that they are not broken, and it’s perfectly OK and critically important to address and even train problematic areas. We are not as fragile as we think, and exposing the body to an appropriate level of stress is crucial to psychological and physiological improvements. Usually, this is best accomplished under the direction of a qualified medical or fitness professional.
If you are an avid golfer who currently does not have injuries, it’s a good idea to take a proactive approach. Basic strength & conditioning principles go a long way to reducing the likelihood you have to spend time on the sidelines, or playing through pain. Of course there is also huge performance benefits. More mobile and powerful swings resulting in increased club head speed, and more energy during rounds being the most obvious.
Huge thank you to Patrick Carroll MSc, BSc (Hons) MISCP of Old Quarter Physiotherapy, Cork, Ireland for his help with this article.

Mike Carroll has a BSc in Sport & Exercise Science from the University of Limerick, and is an accredited S&C Coach with the UK strength and Conditioning Association and TPI Fitness Level 3 Certified. He works with golfers of all levels, in individual and group settings. Currently based in Hansen Fitness For Golf, Irvine, CA.
Twitter: @fit_for_golf
Facebook: Fit For Golf Cork
For more from Mike Carroll of Fit For Golf or to get in contact, visit his website www.fitforgolf.blog
References:
-
Murray et al (2017) The Relationship Between Golf & Health: A Scoping Review (LINK)
-
Dye (2005) The Pathophysiology Of Patellofemoral Pain (LINK)
-
Glasgow et al (2015) Optimal Loading: Key Variables & Mechanisms (LINK)
-
Khan & Scott (2009) How Physical Therapists Prescription Of Exercise Promotes Tissue Repair (LINK)